Knowledge Center
January 11, 2022
Today's SPD Guide to Washing and Decontamination Medical Equipment
What Do CSSD and SPD Stand For?
CSSD stands for Central Sterile Services Department or Central Sterile Supply Department, also known as the Central Service Department (CSD). Today, CSSD is still used in Europe; however, most facilities in North America refer to this department as the Sterile Processing Department (SPD).
The History and Evolution of the Central Sterile Services Department
Sterilization of medical devices started with the goal of reducing infections. Surgeons were often responsible for the cleaning and sterilization of their surgical instruments which were sterilized in the operating theater. In 1928, the American College of Surgeons realized that this was not the safest place for decontamination and sterilization of the instruments, and they recommended processing be moved out of the surgical theater. A specialized department was created to centralize all device reprocessing from multiple operating rooms and with this shift, central sterilization departments were born.
The Most Common Equipment Found in A Modern SPD
Today’s sterile processing departments are responsible for the cleaning, sterilization, preparation, and packaging for surgical instruments and medical devices. Equipment common to a SPD include:
| Decontamination "Dirty Side" |
Prep-and-Pack & Sterilization "Clean Side" |
|---|---|
Single-use, consumable items that play a role in the disinfection and sterilization process are also found in the SPD:
| Decontamination "Dirty Side" |
Prep-and-Pack & Sterilization "Clean Side" |
|---|---|
With the volume of cases in today’s healthcare facilities, the management of important record keeping and tracking of instruments is often done using technology to aid in workflow management, asset tracking, and documentation:
| Used across both Decontamination & Sterilization |
|---|
Click to Download the Full Infographic
Medical Decontamination Sinks
Decontamination sinks are used for manual cleaning of medical devices and surgical instruments. Staff using decontamination sinks must follow a multi-step process that involves immersing the device in a cleaning solution and using a physical action to wipe, brush, and/or flush the device.
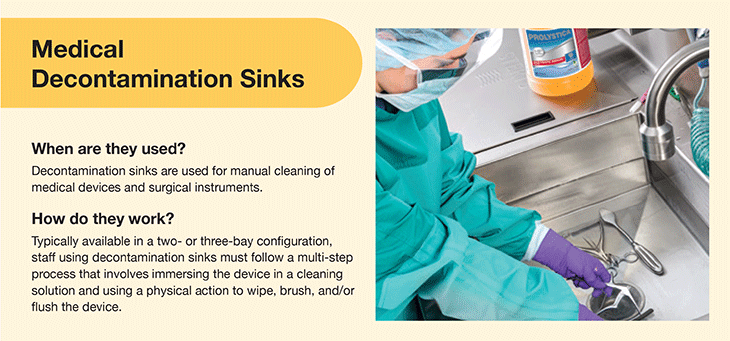
When are Medical Decontamination Sinks Used in the CSSD?
Manual cleaning in a decontamination sink is typically the first step for reprocessing devices in the SPD. Manual cleaning is performed on all instruments but may be exclusively recommended for delicate or complex devices such as drills, endoscopes, or microsurgical instruments. Many instruments require disassembly or specific manual cleaning steps, as stated in the device manufacturer’s instructions for use (IFU).
How Do Medical Decontamination Sinks Work?
For manual cleaning, a three bay configuration is recommended. When using a three bay configuration:
- The first sink bay will have instruments being pre-rinsed with cold water to remove any pre-treatment product or blood.
- The second bay will have instruments immersed and pre-soaking in an enzymatic or neutral detergent solution, then manually brushed using instrument cleaning brushes. When a manufacturer's IFU recommends immersion of the device, cleaning in the sink should be done under the water line to prevent exposure to microorganisms and aerosol generation, especially when brushes are used to clean lumens. The cleaning detergent should be low-foaming so staff can see clearly into the sink to identify all instruments and prevent injuries from sharp objects.
- The third sink bay is used for the final treated rinse. Depending on the manufacturer's recommended practices or a facility's standards, the final rinse should be of a certain quality to help reduce any risk to a patient of a device. Examples include controlled levels of water hardness (to prevent spotting), chloride (to prevent device damage) and microorganisms (to prevent cross-contamination).
Pro Tip for the Modern CSSD
Always follow the device manufacturer’s IFUs to ensure that devices are properly cleaned.
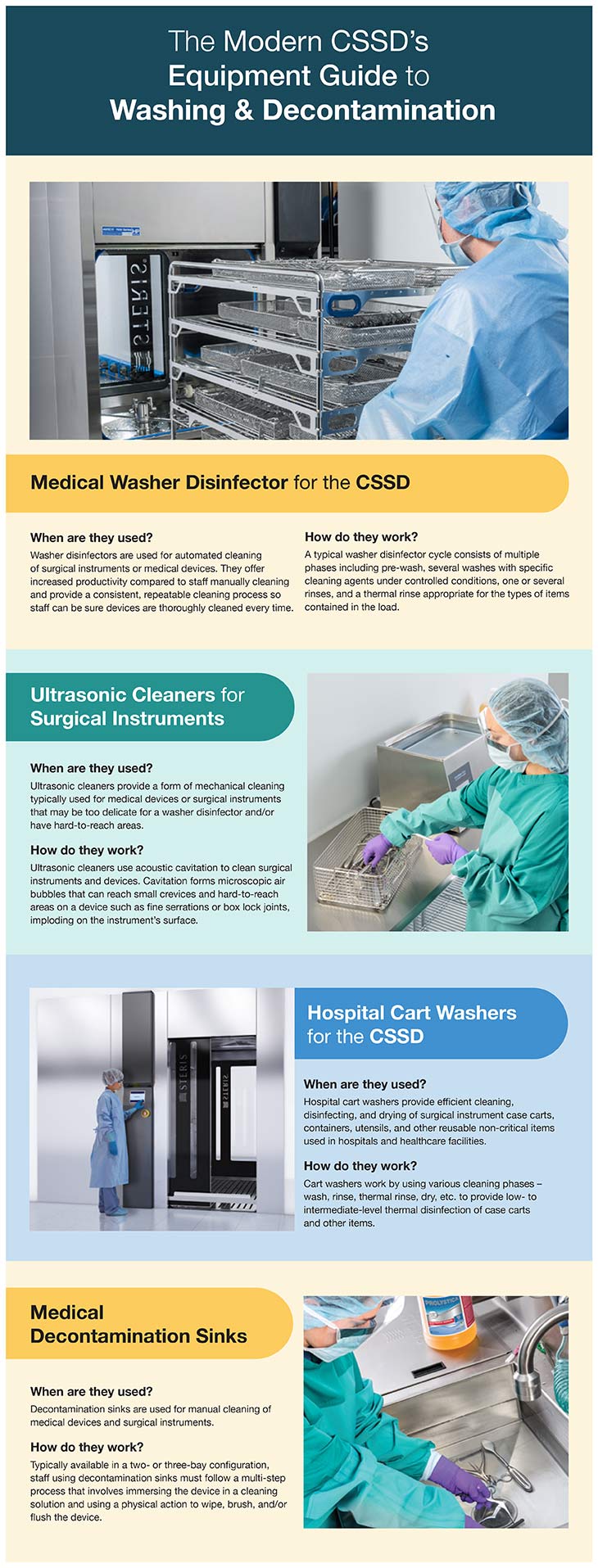
Medical Washer Disinfector for the SPD
Washer disinfectors are used for automated cleaning of surgical instruments and work by combining impingement, water temperature, and detergent to clean heat-resistant and heat-sensitive devices. Advantages of using a washer disinfector for an automated cleaning process are consistency, productivity, and control of essential parameters such as temperature, chemistry, and time.
For both manual and automated processes, key process controls should be in place. The equipment manufacturer and the facility have responsibilities to ensure a safe and effective cleaning process. For an automated washer disinfector process, process control examples include:
- Equipment maintenance
- Detergent use
- Water quality
- Cycle print-out inspection
- Staff competency and training
- Device inspection
When are Washer Disinfectors Used?
The decontamination phase of processing medical devices is a multi-step process. After manual cleaning, most devices are then cleaned and disinfected through an automated washer/disinfector process. The cleaning in an automated washer/disinfector increases productivity while providing a consistent, repeatable process to ensure devices are thoroughly cleaned each time.
After loading the chamber, users will run pre-programmed cycles validated by the original equipment manufacturer (OEM). Custom cycles generally should not be used unless re-validated and cleared for their intended use. After processing in an automated washer, devices are not sterile but are disinfected and generally safe to handle. Washer disinfectors need to be maintained and serviced regularly by trained technicians to ensure their safe and effective use.
How Do Washer Disinfectors Work?
A typical washer disinfector cycle consists of multiple phases:
- Pre-wash
- A washing cycle with specific cleaning agents under controlled conditions
- One or several rinses depending on the cleaning chemistry used
- Thermal rinse which provides disinfection
Pro Tip for the Modern Sterile Processing Department
Many modern washer disinfectors are designed with features that meet national and international standard requirements and improve efficiency and safety. These features may include:
- Independent process monitoring that provides intelligent, real-time feedback
- Documentation and traceability
- Drainability
- Temperature and chemistry distribution
- High Efficiency Particulate Air (HEPA) filtration
- Water, chemical, and energy usage efficiency
- Faster cycle time
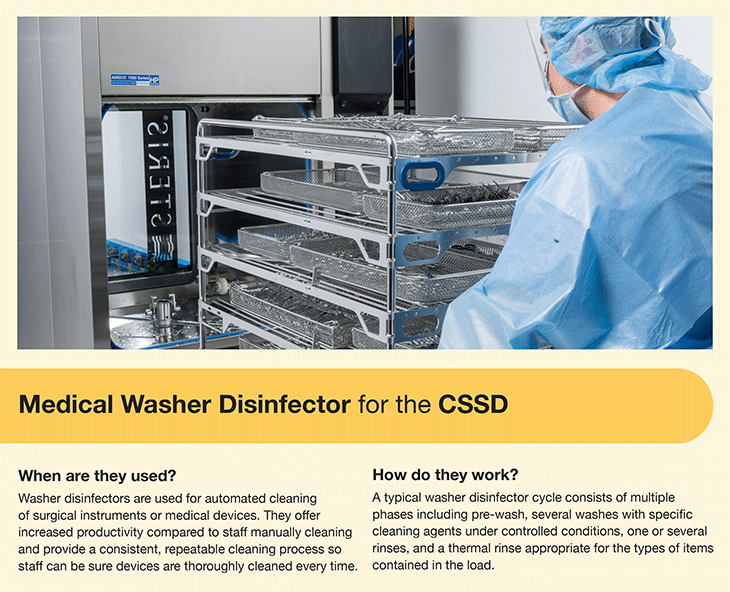
Ultrasonic Cleaners for Surgical Instruments
After manual cleaning, ultrasonic cleaners provide automated cleaning for instruments that may be too delicate for a washer disinfector and/or have hard-to-reach areas. Ultrasonic cleaners use a combination of three parameters to provide effective cleaning: cavitation, flow/sonic irrigation, and cleaning chemistry.
When are Medical Ultrasonic Cleaners Used?
Ultrasonic cleaners are typically used for cleaning delicate and difficult-to-clean semi-critical and critical devices such as minimally invasive surgical (MIS) instruments, laparoscopic devices, robotic surgical attachments, microsurgical and ophthalmology devices.
How Do Medical Ultrasonic Cleaners Work?
Ultrasonic cleaners use acoustic cavitation to clean surgical instruments and devices. Cavitation forms microscopic air bubbles that can reach small crevices and hard-to-reach areas on a device such as fine serrations or box lock joints, imploding on the instrument’s surface. The process is also gentle enough for cleaning delicate items such as microsurgical and ophthalmology devices. Traditionally, ultrasonic cleaning systems have a frequency of 40kHz. However, higher frequency or even dual frequency systems can provide greater cleaning efficacy for the exposure time.
While there are no specific standards on the use of ultrasonic cleaners, industry guidelines advise:
- All gross soil should be removed from instruments prior to placing in the ultrasonic cleaner.
- The ultrasonic cleaning unit should have a cover to contain aerosols.
- Generally, it is recommended to use cleaning agents specifically formulated for ultrasonic cleaners that are low foaming.
- It is essential to manually rinse the device following ultrasonic cleaning unless this is specifically included as part of a validated cycle in an automated process (preferred).
- The cleaning solution should be changed frequently based upon the volume of instruments being cleaned; it is preferred to change the detergent following each use. The unit should be emptied, cleaned, rinsed, and dried on at least a daily basis.
- Instrument sets should not be stacked.
- Each time the water is changed in the unit, the water needs to be "de-gassed." This requires running a cycle with just the metal basket (no instruments) inside.
Pro Tip for the Modern CSSD
Depending on the specific process and device, items made of cork, glass, rubber, wood, and chrome may not be placed into an ultrasonic cleaner. Delicate or microsurgical instruments should only be placed into the ultrasonic cleaner if it follows manufacturer recommendations because the cavitation process can damage the components of delicate devices.
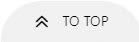
Hospital Cart Washers for the SPD
Hospital cart washers provide efficient cleaning, disinfecting, and drying of surgical instrument case carts, containers, utensils, and other reusable non-critical items used in hospitals and healthcare facilities.
When are Hospital Cart Washers Used in the SPD
Hospital cart washers are used in SPDs to automate the cleaning process and provide low- to intermediate-level thermal disinfection for stainless steel case carts, wire supply carts, tote bins, basins, and rigid sterilization containers. Some cart washers offer an instrument cycle and are validated to wash and disinfect specific surgical instruments. If the cart washer has this instrument cycle, the washer should be tested at least weekly, preferably daily, on the instrument cycle program. Manufacturer Instructions for Use (IFUs) should be followed for processing medical devices that are validated to be cleaned in your specific model/type of cart washer.
How Do Hospital Cart Washers Work?
Cart washers work similarly to single chamber washer/disinfectors and use various cleaning phases such as washing, rinsing, a thermal rinse, and finally drying to provide low- to intermediate-level thermal disinfection. Cart washers can use low or high impingement with the addition of a chemical solution to dislodge soils from the surfaces of these items.
Key Takeaways
In clinical practice, it’s important to remember that cleaning (manual, automated or a mixture of both) is at least a two-step process: cleaning and rinsing. Cleaning can be done manually in a decontamination sink or an automated system like a washer disinfector. All cleaning methods should be controlled or standardized as a process to include any pre-soaking, active cleaning steps, times, temperatures, chemistry dosing, etc. Rinsing, often underestimated, should ensure that all harmful residues including chemicals and residual soils are removed.
Effective cleaning of medical devices is a key step in the processing cycle. If devices are not properly cleaned, sterilization methods such as steam sterilization or low temperature sterilization may not be effective. Learn more about cleaning, sterilization, and sterility assurance in our article "What is Sterile Processing."