Knowledge Center
November 19, 2021
The Complete Guide to a Polypectomy
A colon polypectomy procedure is the removal of polyps (abnormal growth of tissue) from the lining of the colon. In this article, learn more about the different types of polypectomy procedures, techniques, tools used to remove polyps, and screening tests.
What is a Polypectomy?
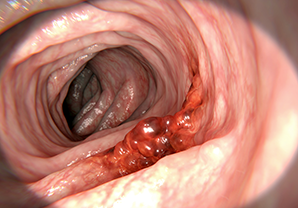
A polypectomy is the removal of a polyp from inside the colon. These procedures are typically minimally invasive and can be performed by gastroenterologists or colorectal surgeons. During a colonoscopy, polyps are identified through the use of a colonoscope. A colonoscope is a long, thin, flexible tube with a camera and light at the end which helps to visualize the colon. If polyps are identified, the endoscopist will usually remove them during the colonoscopy. The endoscopist will decide how to remove the polyp based on what kind of polyp is found.
Types of Polypectomy Procedures
Colon polyps are one of the most common types of polyps found in the body, with more than 40% of individuals over the age of 50 having precancerous colon polyps.1
What are Polyps?
A polyp is an abnormal tissue growth on a mucous membrane. These are usually benign (noncancerous) but can turn to cancer if not removed.2 Individuals with colon polyps often do not have symptoms, stressing the importance of regular colonoscopy exams for individuals over the age of 45.
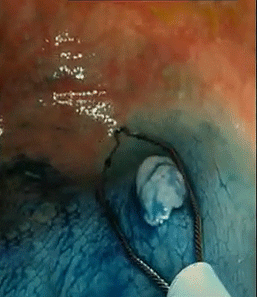
Just as polyps can vary in location, they can vary in size, shape, and type. Polyps are mostly small and round but can also be flat, bumpy, multiple polyps grouped together, or on a stalk-like a mushroom (pedunculated).3
Colon Polypectomy: Types of Polyps
Colonoscopy with polypectomy is a very common procedure. While polyps found in the colon can arise spontaneously, there are common risk factors such as family history, age, excessive smoking or alcohol use, obesity, and other conditions affecting the intestinal tract.4 Oftentimes, patients exhibit no symptoms; however, some polyps can cause abdominal pain, blood in the stool, or changes in digestion. The American Cancer Society recommends that people at average risk of colorectal cancer start regular screening at age 45.5 Colonoscopies are recommended in 10-year intervals, but they may be recommended more frequently if risk factors are high.6
There are two types of colon polyps – neoplastic (includes adenomas and serrated) and nonneoplastic (includes hyperplastic and inflammatory).
- Neoplastic polyps include adenomas and serrated polyps. Adenomas are one of the most common types of polyps. This abnormal tissue can grow out from the colon wall or lay flat on the mucosal tissue. If an adenomatous polyp becomes cancerous, it is known as adenocarcinoma.7Serrated polyps can be large or small. Smaller serrated polyps are typically benign; however, once they progress in size or shape, they are more likely to become malignant.3
- Nonneoplastic polyps include hyperplastic and inflammatory polyps. Hyperplastic polyps rarely turn into cancer. However, if hyperplastic polyps are not removed, or the polyps are large, the risk of turning into cancer increases. These polyps begin as a small growth, usually less than five millimeters in size. They develop as a result of a failure of mature cells to shed normally.8 Inflammatory polyps are related to a patient’s pre-existing inflammatory bowel disease, such as Ulcerative Colitis or Crohn’s Disease. These polyps develop as a reaction to chronic inflammation in the colon. Inflammatory polyps are typically benign.3
Colon Polypectomy Techniques
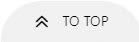
During a colonoscopy, clinicians will use a variety of endoscopic tools to remove a polyp. The technique and tools used for removal are dependent on the polyp size, shape, and location. Polypectomy techniques are typically classified into two types: cold snare polypectomy and hot snare polypectomy. Cold snare polypectomy is commonly used for the removal of smaller polyps. A clinician will use a snare (a wire loop) to surround the polyp and close the device until the polyp is removed. In hot snare polypectomy, clinicians also use snares but during the removal, electrosurgery will be used. View more information on the guidelines for the removal of colorectal lesions.
Clinicians will use a variety of tools during polypectomy procedures. Endoscopic polypectomy tools include:
- Snares – Polypectomy snares are used to remove a variety of lesions. The selection of a polypectomy snare will vary based on polyp size, shape, and location. For example, the Exacto® Cold Snare supports cold snare polypectomy techniques and features a shield shape to resect a variety of small, diminutive, and large polyps. For polyps of various types, the CoinTip™ Snare offers three shapes – deltoid, hexagonal, and diamond – and three size options – 20mm, 10mm, and 6mm.
- Forceps– During a polypectomy procedure, forceps can be used to help obtain a tissue sample. For example, the Centra™ Disposable Biopsy Forceps work with a flexible endoscope to get tissue samples with a variety of jaw sizes.
- Retrieval Net Devices– While commonly used to remove foreign bodies, retrieval nets can also be used during polypectomy procedures to remove the polyp after it has been cut off. These devices also come in a variety of shapes, sizes, and strengths to help retrieve tissue or foreign bodies based on the size and shape of what needs to be removed. Roth Net® Tissue Retrievers help to extract polyps and maintain the sample for further analysis.
- Polyp Traps– Polyp traps, like the eTrap® Polyp Trap, are also used to retrieve resected polyps and lesions that are small enough to be suctioned through the endoscope channel.
- Hemostatic clips– Primarily used for endoscopic hemostasis, clips such as the Assurance™ Clip and Padlock Clip® Defect Closure System can be used during complex polypectomies such as Endoscopic Mucosal Resection (EMR) to help facilitate defect closure, endoscopic marking and anchoring.
- Needles– Injection needles are designed to be used for the injection of various types of media through flexible endoscopes. They can also be used for injection-assisted polypectomies to lift lesions from the muscle layer (muscularis) to improve safety and reduce the risk of perforation during resection.
Colorectal Cancer

Colorectal Cancer Screening
A colonoscopy is the main method for colorectal cancer screening, but there are other options that differ in how often adults should be screened. Visual (structural) examinations, which include colonoscopy, computed tomography colonography (CTC), and flexible sigmoidoscopy (FS), are recommended screening methods anywhere from 5-10 years, depending on which option is selected. Stool-based screening tests are usually recommended to be done between one and three years depending on which test is selected.10
Types of Polypectomy Screening Tests
There are two common polypectomy screening tests for colorectal cancer - a visual exam (colonoscopy) or a stool-based test. As with any procedure, there are potential risks or complications associated with colonoscopies. Potential risks of colon screening tests include:11
- Perforation
- Splenic Injury
- Postprocedural Bleeding
Visual exams (Colonoscopy) typically require less frequent screening compared to stool-based tests. A colonoscopy will allow the doctor to see the full colon (large intestine) and remove polyps during the procedure. Stool-based screenings have fewer immediate risks because they are not invasive. Stool-based tests help to reduce the need for repeated screenings but are less effective for advanced adenoma detection. These screenings may be less expensive than visual examinations, can be done at home, and sometimes do not require diet or medicine restrictions prior to the test.10 However, there is a risk of false positives or false negatives with the use of stool-based tests.
Overview of a Colorectal Cancer Pathology Report
Once polyps are removed during a colonoscopy, the tissue samples will be sent to pathology for review. Pathology reports provide insight into the type of polyp and additional treatment, if necessary. Information typically contained within a colonoscopy pathology report includes:
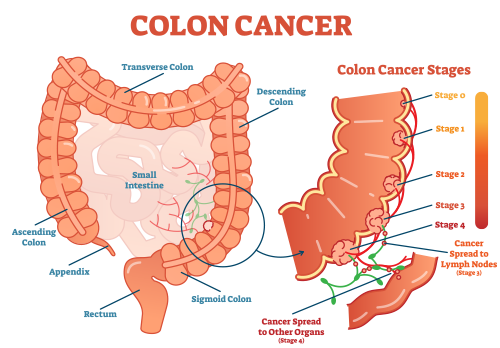
- Location information– The report will provide insights as to where the polyps were found within the colon. For example, ascending, descending, and sigmoid are all parts of the colon.
- Growth pattern of the polyp– Pathologists will exam the growth patterns of the tissue to determine the type of polyp, whether neoplastic or non-neoplastic. In addition to determining if the growth is cancerous, examining the formation of the polyp helps to determine the path forward when it comes to ongoing screenings and tests.12
- Type of polyp– The pathology report will determine the makeup of the polyp tissue. An adenoma is a type of polyp growing in the colon. There are several different types of adenomas, and cancer can start as an adenomatous polyp. Adenomas have two common growth patterns, tubular (common in smaller adenomas) and villous (common in larger adenomas).
Once a mass is determined to be cancerous, the report will determine the stage of cancer – from Stage 0 to Stage 4 – depending on the progression. The American Joint Committee on Cancer uses a TNM system to determine the stage of cancer. The T stands for Tumor, investigating where the tumor is growing and how it is growing. The N stands for Node and involves determining if the tumor has impacted the lymph nodes. Lastly, M stands for Metastasis, where doctors examine the rest of the body to see if cancer has spread anywhere else.13
Colorectal cancer can also be described by its grade. The grade is determined by how many cancer cells look healthy when a doctor views them through a microscope. If the grade of the cancer is lower, that will result in a better prognosis. The doctor may also be able to predict how fast cancer will spread depending on the cancer’s grade.14
When determining the survival rate for colorectal cancer, cancer is analyzed based on three different categories that the SEER database (maintained by the National Cancer Institute) recognizes.15 These categories are localized, regional, and distant. Localized means cancer has not spread anywhere else in the body. In the case of colorectal cancer, regional means cancer has spread from outside the colon/rectum, but only to nearby structures. Distant means cancer has spread to different parts of the body that are further from the colon.
Looking at data from SEER (Surveillance, Epidemiology, and End Results Program), the following numbers are from people diagnosed with colon cancer between 2010 and 2016:15
- Localized: 91%
- Regional: 72%
- Distant: 14%
The following numbers are from people diagnosed with rectal cancer between 2010 and 2016:
- Localized: 89%
- Regional: 72%
- Distant: 16%
Colorectal Cancer Treatments15
Based on how advanced the cancer is, there are different treatments options. If the cancer is in the early stages, there are minimally invasive procedural options to remove the cancerous polyp. Some of these include polypectomy, EMR (Endoscopic Mucosal Resection), ESD (Endoscopic Submucosal Dissection), or laparoscopic surgery. If the cancer is in a more advanced stage, the doctor may recommend surgery such as a partial colectomy and/or lymph node removal.
If the cancer is too advanced to have surgery, or the risk is too high for surgery, other treatments for colorectal cancer include:17
- Chemotherapy
- Radiation therapy
- Targeted drug therapy
- Immunotherapy
- Palliative care
polypectomy procedures takeaway
A polypectomy procedure is the removal of a polyp from inside the colon. This article covered the different types of polypectomies, colorectal cancer screenings, and how colorectal cancer is detected.
Article References
1 https://www.asge.org/home/for-patients/patient-information/understanding-polyps
2 https://www.cancercenter.com/prevention/what-are-polyps
3 https://www.uofmhealth.org/conditions-treatments/digestive-and-liver-health/colon-and-rectal-polyps
4 https://www.mayoclinic.org/diseases-conditions/colon-polyps/symptoms-causes/syc-20352875
7 https://medlineplus.gov/ency/article/000266.htm
8 https://www.healthline.com/health/hyperplastic-polyp#treatment
9 https://clinicaltrials.gov/ct2/show/NCT02717598
10 https://acsjournals.onlinelibrary.wiley.com/doi/full/10.3322/caac.21457
13 https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/staged.html
14 https://www.cancer.gov/about-cancer/diagnosis-staging/prognosis/tumor-grade-fact-sheet
15 https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/survival-rates.html
16 https://www.cancercenter.com/cancer-types/colorectal-cancer/treatments/surgery
17 https://www.cancer.org/cancer/colon-rectal-cancer/treating/by-stage-colon.html