Knowledge Center
January 11, 2022
How are Surgical Instruments Cleaned and Disinfected?
Surgical instruments and other reusable devices must be effectively reprocessed so they are safe and functional for patient use. Before an instrument can go through sterilization or high-level disinfection, it must be cleaned. To ensure quality outcomes for the patient, the cleaning process requires consistency and standardization.
Before reviewing the details of the process, it's important to understand the distinction between "cleaning" and "disinfection." Here are a few key definitions to know:
- Visible Soil: Blood, bone, tissue, and inorganic soils such as dirt or dust
- Non-Visible Soil: Microorganisms, bacteria, and viruses or chemicals
- Cleaning/Decontaminating: The removal of contamination (often referred to as "soil") from a surface to the extent necessary for further reprocessing or the intended use of the surface. (ANSI/AAMI/ISO 15883-1)
- Disinfection: The antimicrobial reduction of the number of viable microorganisms on a product or surface to a level previously specified as appropriate for its intended further handling. Most automated washer/disinfectors will accomplish this through thermal disinfection.
- High Level Disinfection: The elimination of all microorganisms in or on an instrument, except for small numbers of bacterial spores.
- Sterilization: The process to eliminate all viable microorganisms.
Next, let's review the steps in reprocessing surgical instruments starting from point-of-use to manual cleaning and finally automated cleaning using a washer/disinfector or ultrasonic cleaner.
Step 1: Point of Use Pre-Cleaning

The first step in cleaning a surgical instrument is to initiate pre-treatment. Instrument transport gels, like Pre-Klenz™ Point of Use Preprocessing Gel, help initiate the cleaning process of surgical, endoscopic, and robotic instruments immediately after use. Instrument transport gels prevent the drying of bioburden, which can decrease the time needed to manually clean at the sink, as well as loosen soils.
Step 2: Manual Cleaning of Surgical Instruments
After point-of-use pre-cleaning, instruments are transported to the decontamination area of the Sterile Processing Department (SPD) to begin manual cleaning. Manual cleaning should be performed on all instruments but may be recommended as the preferred method of cleaning for delicate or complex devices, such as endoscopes or microsurgical instruments. Devices must be removed from the transportation container and disassembled to expose all the surfaces to the cleaning process. Always follow the device's Instructions for Use (IFU) for comprehensive instructions for cleaning and disassembly.

For manual cleaning, a three bay sink configuration is recommended. When using a three bay configuration:
- The first sink bay will have instruments being pre-rinsed with cold water to remove any pre-treatment product or blood.
- The second bay will have instruments immersed and pre-soaking in an enzymatic or neutral detergent solution, then manually brushed using instrument cleaning brushes. When a manufacturer’s IFU recommends immersion of the device, cleaning in the sink should be done under the water line to prevent exposure to microorganisms and aerosol generation, especially when brushes are used to clean lumens. The cleaning detergent should be low-foaming so staff can see clearly into the sink to identify all instruments and prevent injuries from sharp objects.
- The third sink bay is used for the final treated rinse. Depending on the manufacturer’s recommended practices or a facility’s standards, the final rinse water should be of a certain quality to help reduce any risk to a patient of a device. Examples include controlled levels of water hardness (to prevent spotting), chloride (to prevent device damage) and microorganisms (to prevent cross-contamination).
Step 3: Automated Washing and Disinfection of Surgical Instruments
After manual cleaning, most devices are then processed through automated cleaning technologies such as ultrasonic cleaning systems and washer/disinfectors.
Ultrasonic Cleaning
Ultrasonic cleaning is used for fine cleaning of instruments with hard-to-reach areas like crevices, hinges, and lumens. After manual cleaning, the devices should be sorted based on metal to prevent damage. For example, aluminum instruments can react with stainless steel if immersed together, causing etching, or replating to the devices.

Ultrasonic cleaners work through cavitation where high-frequency sonic waves create tiny bubbles on the surfaces of the instruments which eventually implode. The implosion of these bubbles helps to dislodge soil from the surface of the device. Low-foaming enzymatic cleaners can be used in ultrasonic cleaners, assuming the foam does not interfere with the cavitation process. After the ultrasonic cleaning process, the instruments must be thoroughly rinsed with either deionized or softened water.
Advantages of ultrasonic cleaning include a reduction of time spent to clean complex instruments and removal of residual soil, however not all materials or devices are compatible with this type of cleaning.
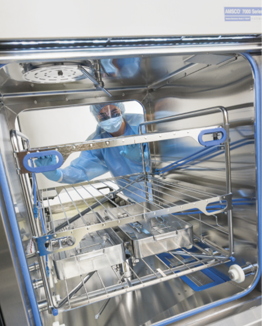
Washer/Disinfectors
The mechanical cleaning action of washer/disinfectors relies on spray arm technology with pressurized water to help clean surgical instruments or other reusable devices. The load inside a washer/disinfector is exposed to a specific water temperature, chemical concentration, and flow rate. The thermal rinse phase in a washer/disinfector provides a level of disinfection. An optional drying phase can be added to reduce manual drying.
Successful cleaning using washer/disinfectors depends on four parameters within the cycle:
- Time – If the cycle is too short, cleaning may not be achieved; however, if it's too long, efficiency is compromised.
- Temperature – The temperature of the cycle wash depends on the validated pre-programmed cycle and cleaning chemistries being used.
• When enzymatic cleaning chemistries are used in washer/disinfectors, they typically work best between 100-140 F/32-60 C with detergents typically being used in ranges between 122-180 F/50-82 C. This can vary by manufacturer.
- Chemistry – The recommended cleaning chemistries are determined by the washer/disinfector manufacturer and the IFUs for the devices being processed. Other factors to consider in selecting a cleaning chemistry are water quality and concentration of chemistry.
- Impingement – Representative of the mechanical force of spray arms. If low impingement washer/disinfectors are used, a more aggressive cleaning chemistry may be needed. High impingement washers rely on the high pressure of the water to aid in soil removal.
Washer/disinfector cleaning offers consistency and productivity, as parameter control is easier. Staff must be properly trained on device loading to ensure effective use.
Cleaning Failures – Residual Soil and Common Causes
If after manual and mechanical cleaning soil is still present, this can present several risks, with the most severe being the risk of transmission to patients. In addition, residual soils left on devices can damage the device's surfaces or ability to function correctly.
Possible Causes of Cleaning Failures
If soils are left on surgical instruments or reusable devices after cleaning, common causes could be:
- Ineffective use of cleaning chemistries – Either the wrong chemistry was used or an incorrect dilution rate
- Assembly of the instrument – The instrument was disassembled incorrectly, which caused soils to become stuck in crevices or lumens
- Issues or failures with equipment – Problems with the mechanical technologies, including misuse (i.e. overcrowding of trays) or equipment failures
- Issues with manufacturer instructions – Instructions are either hard to follow or contradict department procedures
Cleaning Verification and Inspection Methods
After cleaning, all devices should be visually inspected thoroughly with a lighted magnifying glass. In addition to routine visual inspection, there are several methods that can be used to test cleaning efficacy:
- Cleaning Indicators – Cleaning process indicators verify that the washer/disinfector cycle process parameters in all phases have the cleaning cycle have been achieved. The indicator materials will break down or exhibit a color change when the parameters have been successfully achieved.
- Cleaning Verification – Beyond visual inspection, many hospitals use a cleaning verification program such as ATP or Protein detection. Protein is found in almost all surgical soils, and any living organism, therefore detecting it on a "clean" device can help identify gaps in cleaning procedures or hidden damage to devices.
Guidelines for Cleaning and Disinfecting Surgical Instruments
There are a variety of standards surrounding cleaning surgical instruments and medical devices. Governing agencies, including AAMI/ANSI, FDA, and AORN release guidelines for cleaning and disinfection. Specific device IFUs should always be followed to ensure the device is reprocessed according to the manufacturer. The specific standards/guidelines around cleaning are spread throughout many standards, but the most common ones are:
- ANSI/AAMI ST79, Comprehensive guide to steam sterilization and sterility assurance in health care facilities – most commonly referenced because of its detailed washer indicator Appendix.
- ANSI/AAMI ST58, Chemical Sterilization and High-Level Disinfection in Health Care Facilities
- ANSI/AAMI ST91, Flexible and Semi-Rigid Endoscope Processing in Health Care Facilities – because of its focus on the cleaning of complex endoscopy devices
Importance of Properly Cleaning Reusable Devices
Cleaning is an important step in the reprocessing of a reusable device or surgical instrument. Both manual and automated cleaning can be used and the methods will vary based on the device. Cleaning reusable devices is important to prevent what we can see – including device damage – as well as what we can't see like pathogenic microorganisms or transmissible proteins. If devices are not clean, they cannot be properly sterilized, or high-level disinfected.