Knowledge Center
October 2, 2019
The Cost of Not Monitoring Every Load

Recalls of a sterilization load are a possibility your department must be prepared for and are a lot like car repairs. They never happen when it's convenient and can end up costing you more than expected – impacting both the sterile processing department and the operating room.
American National Standards Institute/Association for the Advancement of Medical Instrumentation (ANSI/AAMI) ST79 states that in the instance of a failed biological indicator (BI) you must recall all loads processed since the last negative BI result1. This means if you only monitor once daily, per AAMI standards for sterilization, you may need to recall all loads processed for that period and up to the last negative biological indicator.
Financial Risk of Not Monitoring Every Sterilization Load
According to Glenn Pennington, Director of Central Services at a large hospital network in New Jersey – recalls can result in more expense for the operating room (OR) than you may initially think.

"We had a recall once due to a failed biological indicator, and the OR stopped for an hour and a half because we didn't have any cameras we could release," Pennington said. When this occurred, Pennington's department was monitoring their hydrogen peroxide sterilizers once daily with a biological indicator. Following recall procedures for sterilization, the result was a recall of devices processed since that failed BI which included cameras that multiple ORs needed.
Besides impacting Sterile Processing Department (SPD) and OR processes, recalls have a measurable cost to your facility. These can include the labor of time spent recalling and quarantining loads, time spent repackaging trays, plus reprocessing costs. What you also need to consider is lost revenue if the OR must stop. Delays like these waste valuable minutes of operating room time – which could cost a hospital $153/minute. Alternatively, below is a comparison of costs associated with monitoring daily:
Assume a facility running four Cycles/Day with four wrapped packs per cycle:
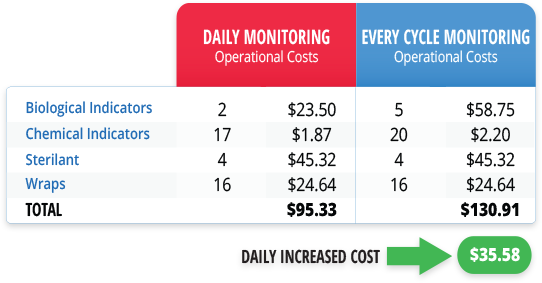
The calculations in this scenario show a marginal increase in daily costs for every cycle monitoring, especially when compared to potential lost revenue from load recalls and the risk of stopping the OR.
The added cost in monitoring every load is like having auto insurance:
is $35 a day worth it to your facility to prevent $9,180 per hour2
in lost operating room time?
How Can You Help to Change your Policy?
When it came time to change their process to every cycle monitoring, Pennington's facility needed approval from multiple stakeholders. “The first step was to run it up to finance, but finance wasn't the only hurdle” said Pennington. “We pulled in the infection prevention team, who were on board right away.” Raising the standard of care became top priority and this easily justified the increased cost related to every cycle monitoring.
Standardizing processes to reduce errors is another key driver to implement every cycle monitoring for hydrogen peroxide sterilizers. Many facilities are already monitoring every sterilization load in steam. At Pennington's facility, standardization was a major factor in switching to monitoring every load – across both steam and vaporized hydrogen peroxide (VHP) processes.

"This has been very helpful – the process is standard!" Pennington said. "If you're pushing something in the sterilizer no matter the unit, you need a BI. We work more efficiently now. Recalls, when they do happen, are not as impactful. We're not stopping the OR because we have a failed biological indicator."
For hospitals unsure about changing to monitoring every load, from Pennington's experience, he asks you to think about one thing: "Think about that process, if you only run one BI a day – just imagine if that one is positive at the end of the day. It can stop the OR," he said.
1 ANSI AAMI ST79 2017 Comprehensive guide to steam sterilization
2 Nichol, P. (2018, December 8). The $49 billion/year of waste in healthcare spending we can solve. Retrieved from https://www.linkedin.com/pulse/49-billionyear-waste-healthcare-spending-we-can-solve-peter-nichol/